Hormones are natural substances produced in the body. Hormones act as “messengers” around the body, which travel through the bloodstream and cause physical and chemical functions and processes within the body to occur.
The ovaries and pituitary glands play significant roles when understanding the female reproductive system. The ovaries make most of the estrogen and progesterone in the female body. Estrogen and progesterone are the two key hormones that control the reproductive system, hence a woman’s fertility. The pituitary gland uses hormones to signal the ovaries to trigger events. Once triggered, the body returns feedback to the pituitary to help the brain regulate these events by reducing or increasing the amount of that hormone released.
To better comprehend what is involved in egg donation, it may be helpful to understand the cycle that the ovaries go through each month.
Starting at the beginning …
Follicles are tiny fluid-filled sacks on the surface of the ovaries, and inside the fluid is an egg. Follicle development is stimulated by the production of follicle-stimulating hormone (FSH). The pituitary gland releases follicle-stimulating hormone. The release of this causes a multitude of follicles to grow on the ovaries. In healthy ovaries, around 15-20 follicles begin to develop. These follicles (those between 2-10 mm) can be counted via ultrasound around day 3-5 of the cycle (Antral follicle count or AFC) and are a prediction of how many eggs could ultimately be aspirated. The pituitary gland continues to release regular amounts of follicle-stimulating hormone until the production of this hormone is suppressed. So, what suppresses the production of follicle-stimulating hormones? Answer: Estrogen and Luteinizing hormone (LH).
Inside the follicles are follicular cells. These follicular cells release estrogen. As the follicles mature, more estrogen is released by the increased number of follicular cells. The increase in estrogen levels sends feedback to the pituitary gland, and it begins suppressing the release of follicle-stimulating hormone. As estrogen levels rise, follicle-stimulating hormone levels decrease. When estrogen levels rise to a specific level, the pituitary gland releases a second hormone: Luteinizing hormone (LH). Luteinizing hormone is released close to mid-cycle. (The peak in luteinizing hormone levels coincides with ovulation.) The increase in luteinizing hormones causes the rupture of the developing follicles on the ovaries, and the egg(s) are released. Many eggs will develop in an egg donor cycle because of the additional hormones. In a natural (non-medicated) cycle, a woman’s body will produce only one dominant egg, and the other follicles will stop developing. When the follicle housing the egg ruptures, the remnants form a temporary organ called the corpus luteum. This organ (corpus luteum) secretes progesterone and estrogen.
The rising progesterone level sends feedback to the pituitary gland, and further release of luteinizing hormone is suppressed. The body now awaits a signal that fertilization has occurred. If no fertilization has occurred, the corpus luteum degenerates, causing a decline in progesterone and estrogen to a lesser extent. The declining estrogen levels (no estrogen produced by the follicular cells or the demised corpus luteum) permit the follicle-stimulating hormone levels to rise again. The decline of progesterone causes the uterus wall lining to shed and precipitates menstruation. We can now circle back to “Starting at the Beginning” above.
There are sometimes references to the follicular and luteal phases of the ovaries. The first half of the menstrual cycle is called the follicular phase. The luteal phase is dominated by the hormones secreted by the corpus luteum.
Follicle Stimulating Hormone (FSH)
Follicle-stimulating hormone is a hormone that stimulates follicles to grow. These hormone levels fluctuate with a woman’s age. Follicle-stimulating hormone is measured on days 2, 3, or 4 of a woman’s cycle. A woman’s menstrual cycle is measured from the first day of her period (blood flow, not spotting), so Cycle Day 3 is the third day of her period. A level under seven is considered normal if the woman is below the age of 34. Follicle-stimulating hormone level below eight is ideal for women from 35 to 38 years old. A level above ten is considered abnormal in all age groups. Low levels are a problem in themselves. Follicle-stimulating hormone levels are suppressed by luteinizing hormone and estrogen. Therefore, low follicle-stimulating hormone levels could indicate that the ovaries are not making enough eggs, the luteinizing hormone and estrogen levels could be overactive, perhaps the pituitary gland is not working correctly, there may be a problem with the hypothalamus, or maybe the woman is very underweight. If the ovaries have many follicles, then the multiple follicular cells will release a more significant amount of estrogen, and a large level of estrogen results in a slowdown in the amount of follicle-stimulating hormone released. As the ovaries age, they release fewer hormones (mainly estrogen, but the ovaries release other hormones). The result is that follicle-stimulating and luteinizing hormones can no longer perform their usual functions to regulate estrogen and progesterone. In such a case, a woman’s body must work much harder to induce ovulation. Fewer follicular cells can release estrogen when few follicles develop, so estrogen levels are lower. Low estrogen will not give feedback to the pituitary gland to suppress the production of follicle-stimulating hormone. Therefore, the release of the follicle-stimulating hormone is not suppressed, resulting in a higher follicle-stimulating hormone level. A high level indicates that the donor may not be eligible to be an egg donor because the quality and quantity of her eggs are low. Two quick qualifications: (1) an elevated follicle-stimulating hormone level does not mean a pregnancy is impossible, (2) ovaries react differently each month, so it is advisable to monitor follicle-stimulating hormone levels for a few months.
Estrogen (E2)
Estrogen is a female sex hormone that is produced mainly in the ovaries. The adrenal glands also produce some estrogen, as do fat cells. Estrogen is responsible for menstruation, menopause, reproduction, sex drive, and bone and blood health. One of the hormones it works in concert with is progesterone, another female sex hormone. Both female and male bodies have this hormone, but females create more. Estrogen is a hormone throughout a woman’s cycle, but the levels fluctuate. The maturing follicle on the surface of the ovaries produces estrogen. At a certain estrogen level, the pituitary gland releases a luteinizing hormone (which facilitates the release of the dominant egg). In addition, the feedback from high estrogen levels causes the pituitary gland to reduce the follicle-stimulating hormone released.
Estrogen levels are checked several times during an egg donor cycle: 1) Part of the day three baseline blood tests and 2) throughout the ovarian stimulation phase of the in vitro fertilization cycle. Sometimes, an estradiol level is checked just before the cycle begins.
If the estradiol level is high on day 3, there is a problem. On day 3 of the menstrual cycle, the follicles have not yet matured, so the body should have low estradiol levels. Remember that estradiol suppresses the release of follicle-stimulating hormones and that once the dominant follicle has reached a good size, the cells in the follicle’s fluid start releasing larger amounts of estradiol. As the estradiol levels increase, the pituitary gland slows down follicle-stimulating hormone production. When estradiol level is at its peak, the pituitary gland is prompted to release luteinizing hormone, which triggers the release of the egg. Therefore, if on Day 3, the follicle-stimulating hormone level is low, but estradiol is high, it could be an indication that the estradiol is artificially keeping the follicle-stimulating hormone level low when, in fact, the follicle-stimulating hormone level is high (which is a bad thing as a high level indicates poor ovarian reserve).
Luteinizing Hormone (LH)
The Luteinizing hormone blood test measures the amount of luteinizing hormone secreted by the pituitary gland once estrogen levels reach a specific high number. In women, luteinizing hormone levels rise mid-cycle and trigger ovulation within 24 to 36 hours. This hormone also triggers the development of the corpus luteum, which in turn produces progesterone. Higher-than-normal levels of luteinizing hormone indicate several disorders, including ovarian failure and polycystic ovary disease.
These three hormones (follicle-stimulating hormone, luteinizing hormone, and estradiol) can all be checked with a simple blood test performed on Cycle Day 3. The average value ranges for the follicle-stimulating hormone, luteinizing hormone, and estradiol tests may vary among different laboratories, so it is important to get an accurate interpretation of the results from your fertility specialist.
Progesterone
The corpus luteum produces progesterone. The corpus luteum is what remains of the ovarian follicle after releasing the egg. Progesterone signals the uterus to prepare for possible implantation. It also signals the pituitary gland to reduce luteinizing hormone production. Interestingly, progesterone also causes a slight increase in body temperature. This change in body temperature can be used to chart a woman’s cycle, i.e., that ovulation has occurred.
Human chorionic gonadotropin (HCG) is produced if fertilization and implantation occur. Human chorionic gonadotropin prevents the corpus luteum from degenerating so that progesterone and estrogen levels remain high. This is the hormone that is used in pregnancy tests. It is also used as the trigger in an egg donor cycle that causes the eggs to mature and helps the ovaries release the eggs approximately 36 hours after the shot (similar to what the luteinizing hormone does in a natural cycle). The timing of the trigger shot is important as the infertility doctor will aspirate the eggs just before the follicles rupture and release the eggs.
Antral Follicle Count (AFC)
An antral (resting) follicle is a small, fluid-filled sac containing an immature egg and can be seen, measured, and counted on Days 2, 3, and 5 using ultrasounds. The number of antral follicles varies from month to month because ovaries behave differently from month to month. Therefore, it is important to do this count before EVERY cycle. Please do not be persuaded by an agency telling you that money can be saved using results from a prior egg donor cycle. Skipping a redo on the follicle-stimulating hormone level testing is okay, but always do an antral follicle count before committing to an egg donor cycle.
A typical mid-30-year-old woman has an antral follicle count of 5-10 follicles per ovary or over 18. Female age and antral follicle count are the best tools to estimate ovarian reserve, the expected response to ovarian stimulating drugs, and the chance for a successful pregnancy. The number of antral follicles visible on ultrasound indicates the number of primordial follicles remaining in the ovary. Each primordial follicle contains an immature egg that can potentially develop and ovulate. When there are only a few antral follicles visible, there are far fewer eggs remaining as compared to when there are more antral follicles. As women age, fewer eggs remain; therefore, fewer antral follicles will be seen on the ultrasound. If the antral follicle count is over 35 (considered a high count), ovarian hyperstimulation syndrome is likely. Sometimes, the ovaries respond poorly to stimulation meds, and very few mature follicles are seen. Generally, the entire cycle is canceled if fewer than three mature follicles are seen on an ultrasound. The problem with an antral follicle count is that it is observer-dependent. One clinician may see eight antral follicles, while another will only see four.
Anti-Müllerian Hormone (AMH)
The Anti-Müllerian hormone is a newer method available to predict ovarian reserve. This hormone is a protein produced by cells in your ovarian follicles, so a high amount of Anti-Müllerian hormone indicates you have plenty of follicles. Therefore, testing a woman’s Anti-Müllerian hormone levels in her blood is another tool to estimate how many eggs a woman has remaining (her ovarian reserve). Unlike other hormones, Anti-Müllerian hormone levels do not fluctuate during the menstrual cycle, so the blood sample can be taken anytime. Women are born with all the follicles they will ever have. Therefore, a woman’s Anti-Müllerian hormone level will not increase with age. This hormone is a good indicator of the quantity of eggs but does not measure the quality of the eggs. Therefore, a high Anti-Müllerian hormone indicates there are lots of follicles and could be an indication of polycystic ovaries (PCOS) or the presence of cysts that do not contain any eggs. It is perfectly possible that there are plenty of follicles containing eggs in addition to the cysts. But there is also a high ovarian hyperstimulation syndrome (OHSS) risk.
The follicle-stimulating hormone level, Anti-Müllerian hormone level, and estrogen level are often called “baseline” and indicate how many egg-containing follicles remain in the ovary. It is super important to remember that while the Anti-Müllerian hormone, follicle-stimulating hormone, Estrogen, and antral follicle count can be a good indicator of how many eggs remain, none clearly indicates the quality of those eggs. The quality of the eggs will be better understood after fertilization when the growing embryos can be examined. While the final determination of the quality of the eggs is a successful delivery, all these tests are tools used by an infertility doctor to evaluate an ovarian reserve and to predict the possible outcome more accurately.
Medical Side Effects of Egg Donation
- Allergic reactions to fertility medications (rarely happen).
- Abdominal swelling, tension, and pressure in the ovarian area.
- Mood swings.
- Bruising at injection sites.
- Temporary menopause-like symptoms, including vaginal dryness and hot flashes.
- Unintentional pregnancy if precaution is not taken due to the enhanced ovulation protocol.
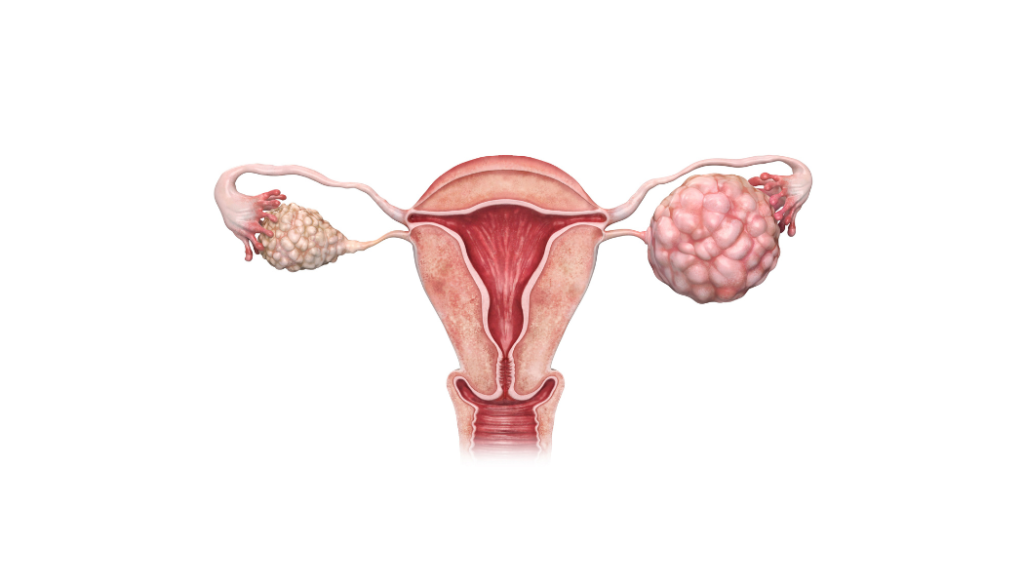
- Adnexal torsion is a condition that results when a stimulated ovary twists on itself and cuts off its blood supply. This rarely happens, but if it does, surgery is required to untwist and, in some cases, to remove the ovary.
- Ovarian hyperstimulation syndrome (OHSS) is a serious complication marked by chest and abdominal fluid buildup and cystic enlargement of the ovaries that can cause permanent injury and even death, dehydration, blood clotting disorders, and kidney damage. If an infertility doctor is concerned about a higher-than-usual risk of Ovarian hyperstimulation syndrome, that doctor may use a Lupron trigger instead of the usual human chorionic gonadotropin trigger for retrieval. A GnRH agonist trigger or Lupron Trigger protocol eliminates the development of Ovarian hyperstimulation syndrome. However, if Lupron is used during the stimulation protocol, it cannot be used as a trigger medication. With modern advances in in vitro fertilization treatment, incidents of Ovarian hyperstimulation syndrome are rarely seen.
- There are reports that indicate that repeated in vitro fertilization cycles can increase the risk of breast or ovarian cancers. Still, recent studies have cast doubt on this and have not shown a clear correlation between stimulating medications and cancer.
Hopefully, this article has demystified the intricate dance of reproductive hormones that orchestrate a remarkable symphony within the female body, governing the menstrual cycle, ovulation, and pregnancy. From the delicate interplay of estrogen and progesterone to the pivotal roles of luteinizing hormone (LH) and follicle-stimulating hormone (FSH), these hormonal forces work in perfect harmony to regulate fertility and maintain the delicate balance of the reproductive system.
Understanding the interplay of these reproductive hormones within a woman’s body can provide valuable insights into the process when participating in IVF.
“I was taught the way of progress is neither swift nor easy.” (Marie Curie)
Author: Karen Synesiou, Infertility Portal, Inc.


