Although it is something we all take for granted, many of us know very little about the complexities of this precious fluid – blood. On average, an adult human body contains approximately 9.5-12.5 pints (4.5 to 6 liters) of blood. Blood makes up approximately 7-8% of an individual’s body weight and is about 50% water. Blood is a living tissue comprised of cells suspended in plasma. It contains red blood cells, white blood cells, and platelets, all crucial in maintaining our health and well-being. The circulatory system pumps about 3,000 gallons (11,356 liters) of blood through the body each day. It travels through a vast network of blood vessels, reaching every part of the body to deliver oxygen and nutrients. If you laid all the blood vessels in a person end to end, they would stretch more than twice the circumference of the Earth!
The components of our blood and their purpose are also fascinating. So, it is worth summarizing some key features to aid your understanding. For example, inside our blood, we have white blood cells (which fight infection), platelets (which help with clotting), and red blood cells (which transport oxygen, remove carbon dioxide, etc.). Blood ‘Antigens’ are the proteins found on the surface of a red blood cell, which determine the kind of antigen you have on your red blood cell.
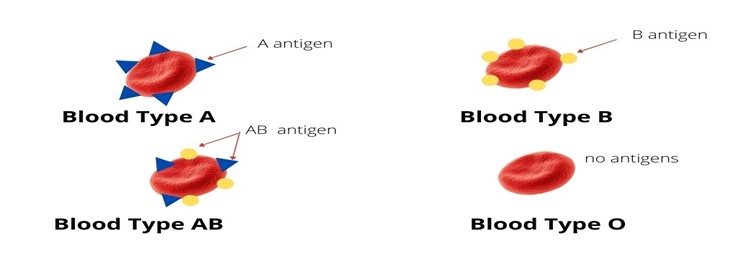
There are four main blood groups (phenotypes): A, B, AB, and O. Some rare blood types fall outside the major groups, e.g., U- RzRz, Jk, Di Kp(b-), etc. In addition to the four main blood groups, we also need to take into consideration a few important factors:
Rhesus factor (Rh): Rhesus factor (Rh) is a significant blood group antigen that can be either positive (Rh+) or negative (Rh-). Rh+ is considered the dominant type, while Rh- is the recessive type. Individuals with Rh-blood type lack the Rh factor, inheriting this from both parents. In contrast, in all other cases, individuals become Rh+ if they receive the Rh factor from either parent.
Understanding the Rh status may be important in Third Party Reproduction. If the individual carrying the baby is Rh+ while the baby is Rh+, the pregnant woman would require two Rh immune globulin injections, such as RhoGAM. Typically, one injection is administered around the 28th week of pregnancy, and the other is given within 72 hours of giving birth. The Rh immune globulin acts as a preventive measure, essentially acting as a vaccine that inhibits the pregnant woman’s body from producing Rh antibodies, which could lead to complications after birth or miscarriage and potentially impact the baby during pregnancy. Therefore, it is essential to be aware of this information to ensure proper medical care and a healthy pregnancy journey.
Co-dominant blood types: A and B are co-dominant or of equal dominance. This means that if the egg contributor has an ‘A’ blood type and the sperm contributor has a ‘B’ blood type, the child will have AB blood.
Blood Type A: A person with type A blood can have two possible genotypes: AA or AO
Blood Type B: A person with type B Blood can have two possible genotypes: BB or BO
Recessive blood type: O is a ‘recessive’ blood type. So, for someone to have an ‘O’ blood type, the egg and sperm contributor must be blood type O. If either donor has a different blood type (A, B or AB), the child will not have blood type O.
Therefore, there are eight possible blood types: A+ A-, B+ B-, AB+ AB-, and O+ O-. Blood type is inherited based on the transfer of the egg and sperm contributor’s genotype to the offspring. (Remember, there are many more blood types, but these rare ones fall outside the major group.)
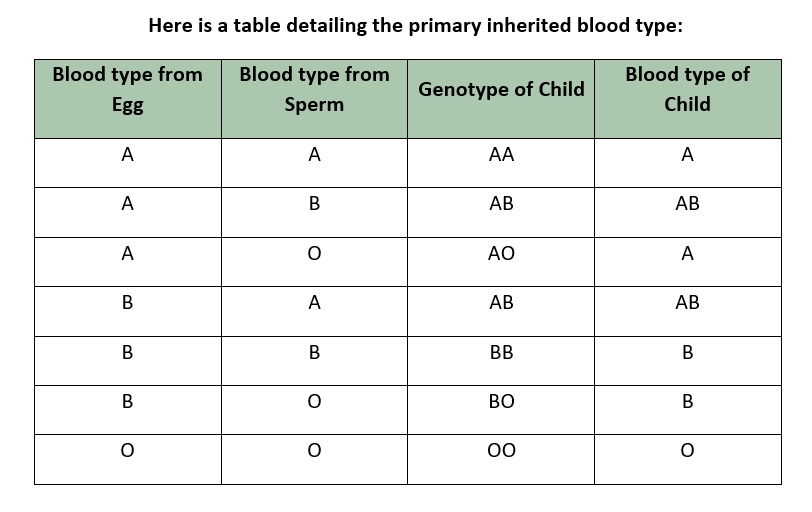
Genotype
So, if you have not nodded off yet and it is not getting too technical, then there is one other aspect to know that’s important – the ‘genotype.’ To understand all the options, a person must know the genotype (i.e., AA, AB, AO, BB, BO, OO) of the genetic contributors and not just their blood type.
Here is an example of why:
If a sperm donor is blood type A and an egg donor is blood type B, they could have a child with blood type A, B or O. In other words, the offspring could be ANY blood type. How is this possible, we hear you ask? The answer lies in the ‘genotype,’ not the blood type.
Example: If the sperm’s genotype is AO (which makes this person blood type A) and the egg’s genotype is BO (which makes this person’s blood type B), then they could have a child with blood type A, B or O. Because the two ‘recessive’ O genotypes could combine and result in an O blood type child.
Example: If the sperm donor is blood type A (with genotype AA) and the egg donor is blood type B (with genotype BB), then the child can only have blood type AB. This is because blood types A and B are ‘co-dominant’, not recessive.
Taking genotypes into consideration, here is an easy-to-understand table of blood types for Offspring:
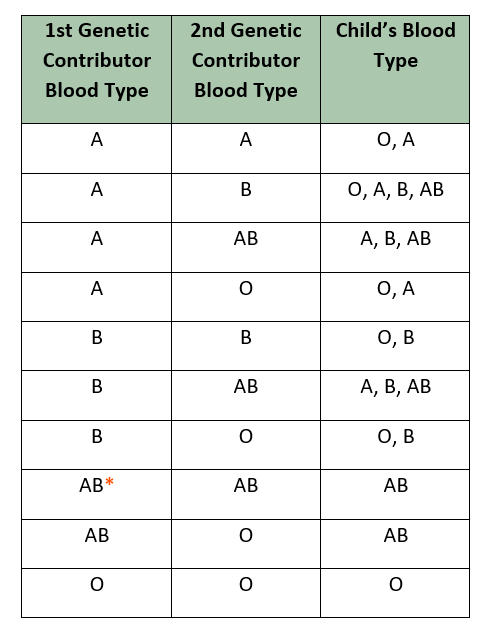
* Note: An AB parent can be a carrier of a rare version of a blood type gene called cis-AB or ABO. If one contributor is ABO and the other O, the child could have an O blood type. This would be an extremely rare occurrence. Another rarity is the Bombay blood type, where people with A or B genes test as an O.
As seen above, matching a donor’s blood type can be complicated, so we typically advocate having a professional agency, expert, or case manager guide you. However, in most cases, blood type does not matter. However, it can prevent potential issues and spare you unnecessary distress if you educate yourself in advance. Therefore, taking the time to become informed about the matter is essential, ensuring you are well-prepared and not complacent about any possible challenges that may arise.
Blood by Ethnicity
Similarly, for some ethnic groups, blood type can be even more important. For example:
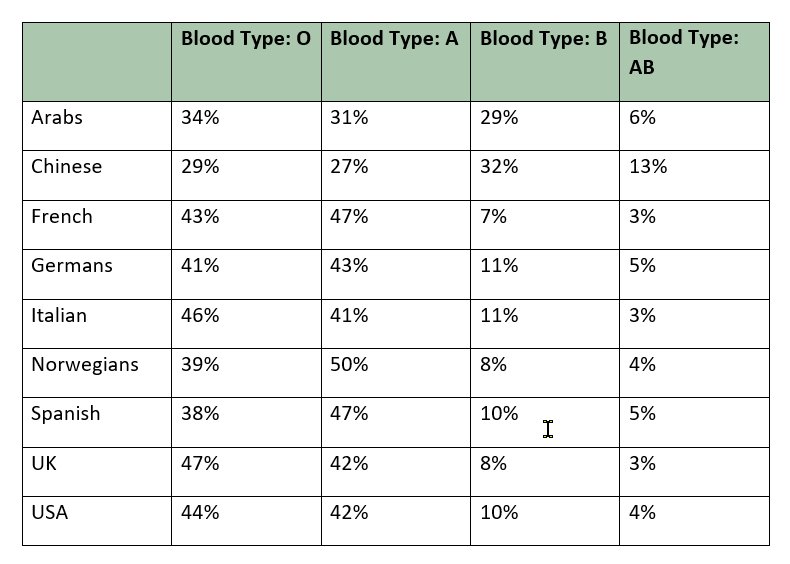
If all of this has you inquisitive for even more information, then there is a really good table on Wikipedia where you can find Blood type distribution by country. This gives you a more detailed dive into blood types by country and ethnicity.
There are also long-term considerations that may need to be clarified. For example, suppose a parent is not ready to reveal their child’s unique genetic beginning. In that case, selecting a donor with a blood type that could be created from the intended parent’s combined blood types may be necessary. Otherwise, there may be an awkward time when they ask why they have blood that is different from yours…
Disclaimer: The information contained herein is NOT intended as medical advice.
CONSULT YOUR DOCTOR TO UNDERSTAND THIS SUBJECT FULLY.
Author: Karen Synesiou, Infertility Portal, Inc.