Endometriosis is derived from the word “endometrium,” the tissue that lines the uterus.
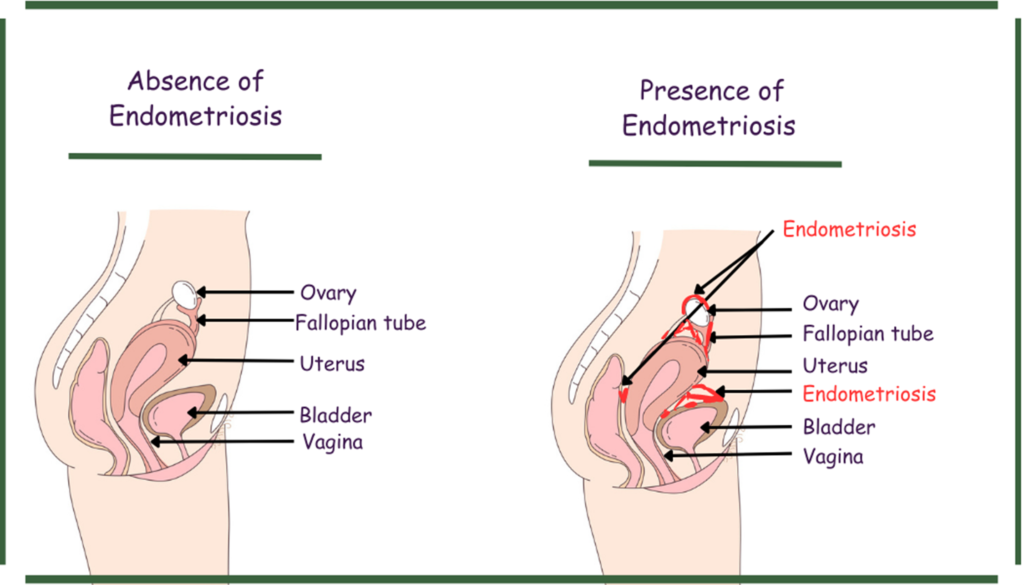
Endometriosis is a medical condition characterized by the growth of endometrial tissue outside the uterus. Typically, the uterus lining, known as the endometrium, regenerates during each menstrual cycle in preparation for a potential pregnancy. However, with endometriosis, this tissue begins to grow in other areas of the body. It can develop around the ovaries, fallopian tubes, and even outside the uterine cavity.
Despite being located outside the uterus, the endometrial tissue associated with endometriosis is affected by hormones like the tissue inside the uterus. It will undergo a similar thickening and breakdown process during each menstrual cycle. However, unlike the healthy endometrial tissue within the uterus that is shed and expelled from the body, the endometrial tissue in these abnormal locations does not get released. Instead, it accumulates and leads to various complications, including inflammation, the formation of scar tissue, the appearance of cysts, and the development of fibrous strands. Sometimes these fibrous strands can cause the reproductive organs to adhere to one another, essentially sticking them together.
Endometriosis is a relatively common condition associated with female infertility, affecting an estimated one in every ten women of childbearing age. Studies conducted by the American Society for Reproductive Medicine (ASRM) have shown that approximately 30-50% of women facing infertility also have endometriosis. The impact of endometriosis on fertility arises from the development of scar tissue surrounding the ovaries, which can disrupt the regular release of eggs or obstruct the egg’s passage through the fallopian tube, preventing its journey to the uterus. Furthermore, endometriosis can cause damage to fertilized eggs, impeding their successful implantation in the uterus. Another consequence of endometriosis is impaired ovarian function, resulting in hormonal imbalances and decreased egg quality.
Causes:
Doctors do not know the exact cause of endometriosis, but here are a few theories of what might cause it:
- Similar to the movement of cancer cells, endometrial tissue may be transported through the blood or lymphatic system.
- After a C-section or surgery, endometrial cells may escape and attach to the wall of the abdomen.
- There is a possibility that endometriosis is a condition that can be inherited.
- One theory is that it’s caused by menstrual blood flowing up through your fallopian tubes and into the pelvic cavity.
- Endometrial tissue accidentally travels into the fallopian tube and into the abdomen instead of exiting the body during a women’s period.
- It is caused by cell mutation.
- It could be linked to hormones.
- It could be linked to a weakened immune system.
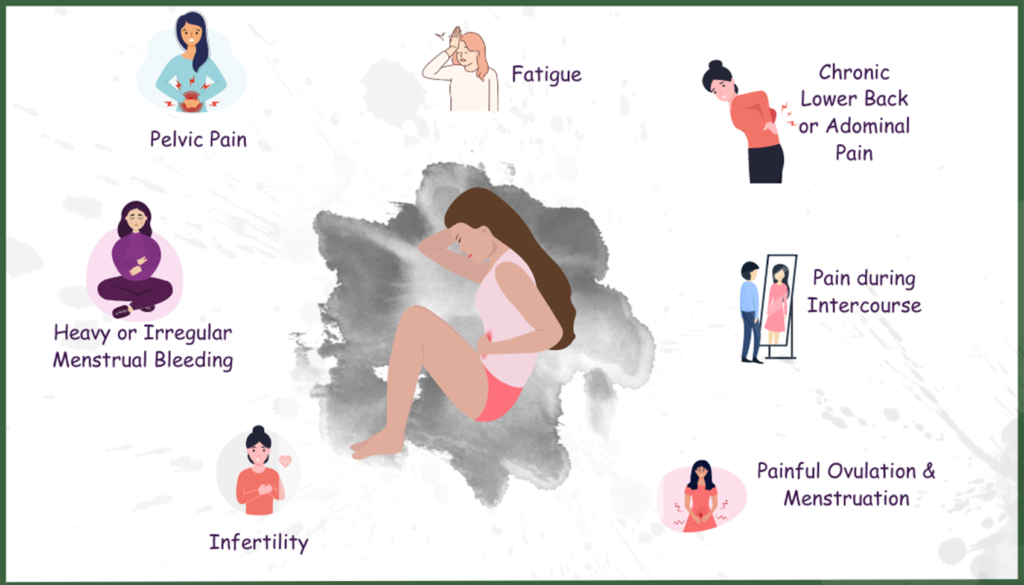
Symptoms of endometriosis may include pelvic pain, excessive menstrual cramps, abnormal or heavy menstrual flow, bleeding between cycles, bloating, pain during intercourse, chronic lower back pain, abdominal pain, feelings of fatigue and nausea, diarrhea or constipation, painful urination, painful bowel movement during menstrual period. Some women will experience no pain, while other women experience chronic pain. Often the symptoms are worsened during the menstrual periods.
Endometriosis is classified into Stages 1 to 4, and each stage is based on where the endometrial tissue occurs in the body, how far it has spread, and how much tissue is seen in each area. Women with endometriosis experience varied symptoms, some with extreme pain and some experiencing no pain. Having severe pain does not equate to more severe endometriosis. Some women with stage 1 endometriosis experience severe pain, whereas those with stage 4 may have few to no symptoms. However, higher stage classification is associated with a higher risk of infertility.
It can sometimes be challenging to know if your feelings are a symptom of endometriosis or “normal” menstrual pain. Even if you feel embarrassed, discussing all the symptoms you experience with your doctor is essential. Keep a note of your symptoms during each menstrual cycle, as this could assist your doctor in detecting a pattern and assist with a proper diagnosis.
Diagnosis
Diagnosing endometriosis is a challenge because the symptoms experienced differ widely. There is no lab test or imaging that can accurately diagnose endometriosis. Unfortunately, surgery is the only sure way of diagnosing endometriosis. However, there are diagnostic options that can identify signs of endometriosis:
- Transvaginal ultrasound involves the insertion of a small wand into the vagina, enabling viewing of the uterus and pelvic area.
- MRI is a noninvasive scan showing the organs and tissue inside the body.
Laparoscopy surgery is the gold standard for diagnosing endometriosis due to its accuracy. Two small incisions around the belly button and lower abdomen are made. Carbon dioxide gas is used to inflate the abdomen. A laparoscope with a light and camera at the end is inserted through one of the incisions. Different areas of the pelvic area can be visualized in real-time. The surgeon will move the laparoscope around the uterus, ovaries, fallopian tubes, and pelvic cavity, looking for signs of lesions, adhesions, and scar tissue. If suspicious tissue is detected, the surgeon will perform a biopsy and extract a small tissue sample for later examination and testing. The surgeon can also evaluate the extent of the endometriosis and rank it from level 1 (minimal) to 4 (severe).
Treatment Options
Treatment options depend on the severity of the endometriosis, the woman’s age, and if she plans to achieve pregnancy. These treatment options all offer relief from the pain of endometriosis. There is a low risk that the endometrial tissue may grow back, and symptoms may return.
- Medications may be administered to control hormones since hormonal changes can cause the progress of endometriosis. This can include oral contraception with estrogen and progesterone to control the menstrual cycle. Progesterone can help stop menstrual cycles and, therefore, endometrial tissue growth. Medication can also be used to suppress the functioning of the pituitary gland and stop menstrual cycles completely.
- Laparoscopy can be used to identify and remove endometrial tissue. Sometimes, intense heat is used to destroy the tissue. Scar tissue can also be removed during a laparoscopy. More invasive surgery involving a larger incision in the abdomen to remove endometrial tissue is another option but is rarely used.
- Surgery to remove the uterus is called a hysterectomy. Another option is the removal of one or both ovaries to stop the release of hormones that cause endometriosis. However, the side effect of this surgery is that it causes the onset of menopause along with hot flashes, bone loss, decreased sexual desire, etc. If the removal of ovaries or a hysterectomy is recommended and the woman is of childbearing age, harvesting and preserving her eggs for later use should be discussed.
Endometriosis can have a profound impact on a woman’s fertility. However, with proper diagnosis, suitable management, and attentive care, women diagnosed with endometriosis can still pursue their dreams of starting a family.
Assisted reproductive services, such as in vitro fertilization (IVF), may be recommended for women with endometriosis experiencing difficulties conceiving. IVF can bypass some of the obstacles of endometriosis and increase the chances of successful conception.
In cases where endometriosis-related complications make pregnancy impossible or medically unsafe, surrogacy can provide an alternative path to parenthood.
Author: Karen Synesiou, Infertility Portal, Inc.