Asthma is a lung disease that causes the airways to narrow, making it hard to breathe. Asthma is a chronic condition. Once you are diagnosed with it, you will have it for the rest of your life. The good news is that asthma can usually be kept under control.
One in 12 adults in America has asthma. Women (9.8%) are more likely to have asthma than men (6.1%). Women have smaller lungs, airways, breathing muscles, and rib cage, affecting airflow, lung volume, and effort required to breathe. In addition, the fluctuations in women’s hormones are thought to affect asthma.
What happens in your body when you have Asthma?
In healthy lungs, the lining of the airways is clear and open, and the muscles surrounding the airways are relaxed. This allows air to flow through freely. With asthma, three things happen—often at the same time—that makes it hard to breathe:
- The airways’ lining gets inflamed, swelling and thickening. This swollen lining narrows the opening so less air can flow through.
- The muscles on the outside of the airways tighten, making breathing the air in and out harder.
- The mucus forms another layer inside the airway, further narrowing the opening.
There are four levels of asthma severity.
- Intermittent asthma – inhaling two or fewer days a week.
- Mild Persistent Asthma – where you use an inhaler more than two days a week, but not daily.
- Moderate Persistent Asthma – where you use an inhaler daily.
- Severe Persistent Asthma – where you are required to use an inhaler several times a day.
Asthma and Pregnancy
Asthma is the most common chronic disease that can cause complications in pregnancies.
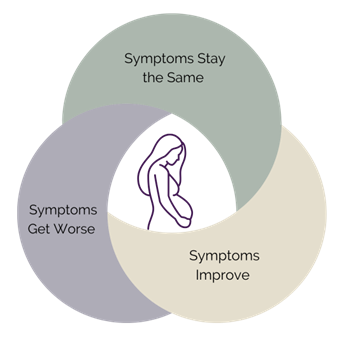
About 1% of pregnant women have asthma. Even if your asthma is well-controlled before getting pregnant, it does not mean it will stay that way during pregnancy. In about 1/3 of women, asthma can worsen during pregnancy, mainly during the first and last trimester. One-third of pregnant women will experience no change in asthma, while a third may even see their asthma improve.
There is no evidence that asthma contributes to miscarriage or congenital malformation of the fetus.
Uncontrolled asthma during pregnancy reduces the oxygen content in the mother’s blood supply. Since the fetus gets its oxygen from the mother’s blood supply, this can lead to decreased oxygen in the fetal blood. Reduced blood supply may impair fetal growth and survival.
The benefits of taking asthma medication during pregnancy are generally believed to outweigh the dangers an asthma attack(s) can cause the unborn baby. Chronically poor control of asthma during pregnancy carries risks, and mothers are more likely to develop complications, including:
- Pre-eclampsia (dangerously high blood pressure)
- Low birth weight.
- A slight increase in the risk of premature birth.
- Increased rate of cesarean delivery.
- Anemia
- Blood clots to the mother’s lungs.
- Obstetric hemorrhage (excessive bleeding before or after delivery)
The good news is that women with well-controlled asthma during pregnancy have outcomes as good as those in no asthmatic pregnant women.
While very few women have asthma symptoms while giving birth, creating a delivery plan with your doctor is advisable. The Australian National Asthma Council recommends regularly reviewing asthma regimes every four weeks during pregnancy.
Avoid Asthma Triggers
The most likely time for an asthma attack during pregnancy is the 24th through 36th week of gestation. Avoiding triggers during this period and continuing to take asthma medication is essential.
- Reduce exposure to pollen, mold, pets, house dust, mite allergy, and strong scents such as paint and perfume. Even cold air can irritate the lungs.
- You should not smoke or vape and avoid second-hand smoke.
- Stay away from people who are sick with respiratory infections. Colds, flu, and sinusitis can make it more difficult for a pregnant woman to manage her asthma. Flu may be particularly severe in pregnant women, so get your flu shot.
- Regular exercise can be beneficial during pregnancy, but check with your obstetrician first. Swimming is an excellent exercise for people with asthma.
Asthma Medications and Pregnancy
There is always concern surrounding the use of any medications during pregnancy. The good news is that most asthma medications are safe for use during this time. Your doctor may change your medicines as some asthma medications are considered safer than others for use by pregnant women. Many mothers-to-be are concerned about taking medications during pregnancy, but the risks posed by uncontrolled asthma are much more significant than those from asthma treatments.
Most importantly, you do not stop taking your asthma medication – especially your preventer. Remember, if you cannot breathe, then neither can your baby!
Keep taking allergy shots/injections if you require them before your pregnancy, but let your doctor/allergist know you are pregnant. You should not start any new allergy medication once you are pregnant.
Work with your doctor to create an Asthma Action Plan for your pregnancy. An Asthma Action Plan is a personalized guide from your healthcare provider. It details what medication you need to take, when to take it, when to adjust them, and what to do if you have a more severe or ongoing asthma attack.
If you experience an asthma attack, your written Asthma Action Plan should show you what to do. If your breathing problems persist or worsen, follow the Emergency section of your written plan and call an ambulance or go to the hospital. Remember to tell the ambulance staff and Emergency staff that you are pregnant. Do not delay seeking medical intervention – it is important to seek help early.
If any of these symptoms are present, you have poor control of your asthma, and you need to contact your doctor or get help immediately:
- Less able to do your usual activities due to asthma symptoms.
- More than one asthma symptom during the night or on waking per week.
- Daytime symptoms more than two days per week.
- Need reliever medication more than two days per week, or the reliever effects only last for 2-3 hours or less. (Reliever relieves coughing and wheezing symptoms and should last 4 hours.)
Women who experience changes in their asthma during pregnancy—either worsening or improving—generally return to their pre-pregnancy asthma levels within three months of birth. Regarding breastfeeding, it is safe to use quick-relief and controller inhalers.
And remember to refill your asthma prescriptions before the birth so you are covered for the first weeks home with your baby.
Author: Karen Synesiou, Infertility Portal, Inc.


