Many different medical conditions and other factors contribute to fertility problems, and often, there is a combination of causes. Overall, one-third of fertility problems are caused by male reproductive issues, one-third by female reproductive issues, and one-third by unknown factors. While 7% of the male population is affected by infertility, sadly, the subject of male infertility is rarely discussed openly, mainly due to social and cultural taboos.
While a woman is born with all the eggs they will ever create, men create new sperm cells every 74 days. The exact time frame differs from person to person. The male reproductive cell is the sperm. The word sperm is derived from the Greek word “Sperma” which means seed and is the smallest cell in the human body. It is a haploid containing 23 chromosomes, half the genetic material required to create a fetus.
While an egg always contains an X chromosome, the sperm can have either an X or Y chromosome. Therefore, the DNA carried by the sperm will determine the sex of the fetus. (XX for female or XY for male).
Spermatogenesis
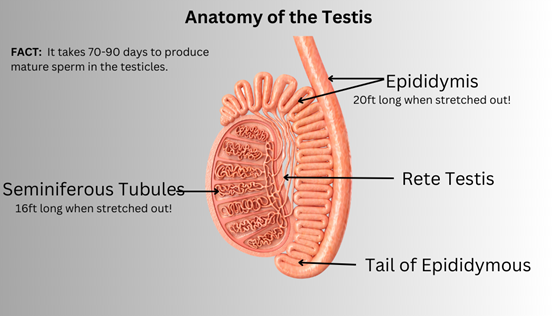
Spermatogenesis is the name given to the process of creating sperm cells. However, the process is sensitive to temperature, so, during puberty, the testicles descend from the body to hang between the legs. This keeps the testis about 4 degrees cooler than the usual body temperature. Each testis weighs approximately 0.875 ounces and is about 1.6 -2 inches in diameter.
The testicles are responsible for making sperm and producing testosterone. Higher and higher amounts of testosterone are produced as boys go through puberty. Testosterone is the hormone that causes boys to develop deeper voices, muscles, and body hair and stimulates sperm production.
Inside each testis are fiber-like strings or tiny tubes called seminiferous tubules. The sperm cells (spermatocytes) are produced within the walls of these tubes.
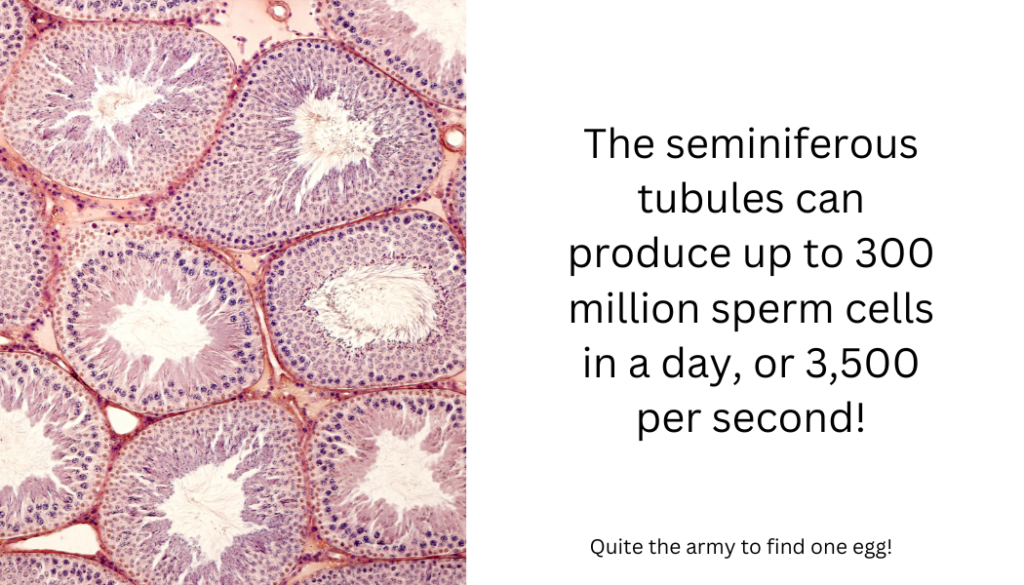
After maturing for 65-75 days, these sperm cells drop into the tube’s hollow “center” (i.e., the lumen) and are moved by involuntary muscle contractions to the epididymis, where they are stored. The epididymis is a tightly coiled tube that, if stretched out, will reach over 20 feet long! Upon entering the epididymis, the sperm cells are immotile and have not yet developed tails. The mature sperm cell then moves along the epididymis and is stored in the epididymis’s tail, where they are released to the vas deferens tube during ejaculation. As the sperm passes through the vas deferens, they pass through various glands, including the prostate. They mix with fluids from these glands and form semen.
Characteristics of Sperm
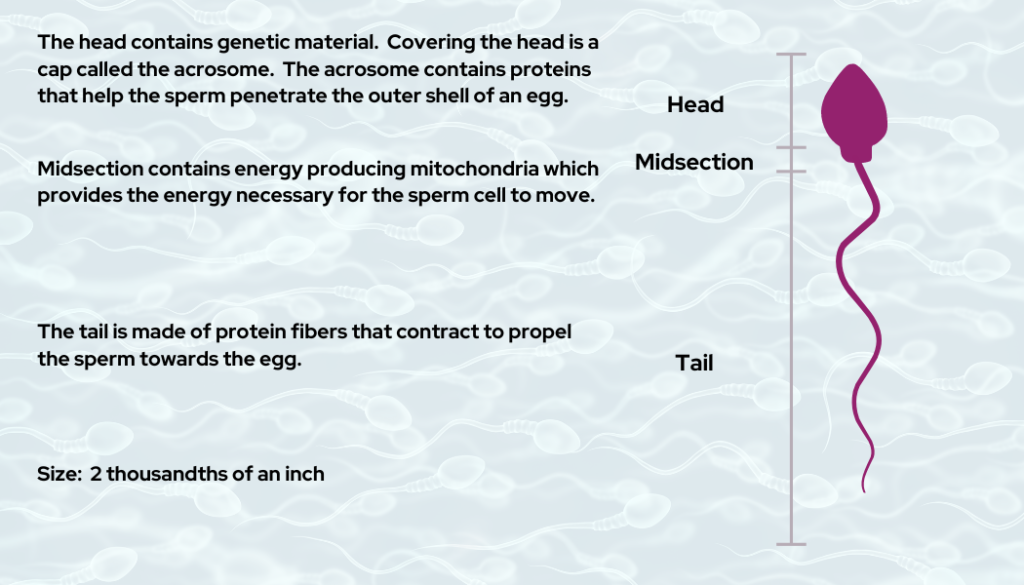
Sperm consists of 3 regions:
- Head
The head section is covered by a cap (acrosome) which covers 40-70% of the head. The acrosome contains the enzymes needed to penetrate the outer membrane of the egg so that fertilization can occur.
The head also contains DNA. i.e., 23 chromosomes are half the chromosomes needed to create a human.
- Midsection
This region stores a few days’ worth of energy needed to keep the sperm alive and provides the energy required for the sperm to move. If the sperm does not fuse with the egg when the energy is depleted, the sperm will die.
- Tail
The purpose of the tail is to create motion that propels the sperm toward the egg. Sperm swim about 30 inches per hour.
Evaluating Sperm
Sperm quality and quantity can be accessed via sperm testing. The most common test to evaluate a man’s fertility is semen analysis. The analysis will include:
- sperm count (number of sperm),
- percentage of moving sperm (motility),
- percentage of normally shaped sperm (morphology).
- the volume of fluid (semen volume).
Fertility clinics generally use two standards in evaluating sperm count: The World Health Organization (WHO) and the Kruger Strict Criteria. Of the two, the WHO criteria are more lenient.
The WHO guidelines consider a healthy sperm count to be 15 million per milliliter or at least 39 million per ejaculation. The guidelines state that 4% and higher sperm having normal morphology is an acceptable composition for fertility.
The Kruger Strict Criteria scoring provides that:
- When over 14% of sperm have normal morphology (normally shaped), there is a high probability of fertility.
- When 4-14% of sperm have normal morphology, fertility probability decreases slightly.
- However, when a sperm sample has a 0-3% normal morphology, fertility is highly impaired.
Sperm can be misshapen such as having two heads, a small head, no head or tail, two tails, a coiled tail, or a stumped tail. An abnormal semen analysis does not mean the person is infertile. Semen analysis results can vary quite drastically from clinic to clinic. It is highly recommended that a semen analysis be undertaken at a fertility clinic and one that runs several semen analyses every day instead of one or two per week.
The average man produces 2.5 -5 mL of semen, which contains between 200 and 300 million sperm, from which less than 10% of the sperm is ranked as normal.
Azoospermia is when there is no sperm present in the semen sample. This condition affects 1% of the male population. Azoospermia is caused by a blockage along the reproductive tract, hormonal problems, ejaculation problems, or issues with the structure or function of the testis. However, there is still a chance of achieving a pregnancy despite the diagnosis of azoospermia with IVF and ICSI (in which a single sperm is injected into the egg, allowing fertilization to occur).
Sperm Collection
Semen samples are usually collected by masturbating into a sterile container at the IVF clinic or doctor’s office. The man is recommended to abstain from releasing sperm for at least two days before collection but no longer than seven days.
Before masturbation, the man should:
- Pass urine.
- Wash hands and penis with soap to reduce the risk of contamination of the specimen with commensal organisms from the skin.
- Rinse away the soap.
- Dry hands and penis with a fresh disposable towel.
- Ejaculate into a sterile container.
If the semen sample is being collected at home, it is essential to get it to the laboratory within 30 minutes of ejaculation for the most accurate results.
The typical steps taken by a laboratory for semen analysis are:
- Measure the volume of the semen in the container.
- Semen pH is measured to determine the acidity or alkalinity of the sample.
- Sperm concentration is taken by measuring the number of sperm contained in a milliliter of semen.
- The total number of sperm in the container is estimated.
- The number of sperm moving in a straight line is noted and will provide the sperm motility measurement.
- Sperm morphology is observed. This is the number of sperm in the sample with a normal shape.
How to increase sperm count?
Because new sperm cells are created approximately every three months, there is the option of improving sperm analysis. Actions today to enhance sperm quality may impact a sperm sample provided 3 or 4 months later.
- Get your hormone levels checked.
- Check for urinary infections, as bacteria in the sperm sample can affect sperm quality.
- Avoid jacuzzi or saunas, as both will increase your body temperature, which is known to kill sperm cells.
- Get enough exercise and sleep.
- Quit smoking.
- Avoid excessive alcohol and drug use.
- Discuss any medication you are taking with your fertility doctor.
- Get enough Vitamin D.
- Some herbal remedies, including taking fenugreek supplements and ashwagandha (Indian ginseng), are considered beneficial. However, no published studies conclude that these herbal remedies increase sperm count. Speak to your fertility doctor before taking any herbal remedies.
- Eat more antioxidant-rich foods. Plant-based foods are the best sources of antioxidants, e.g., fruits (especially blueberries), nuts, spices,
- Limit your intake of soy products, as soy is high in estrogen.
- Your doctor may prescribe medication to treat low sperm count.
An abnormal semen analysis does not mean that a man cannot father a child; it just means it may take longer. Intracytoplasmic sperm injection (ICSI) can be used during an IVF cycle to increase the chance of fertilization. ICSI is when the embryologist selects a normal-looking sperm and directly injects the sperm into the egg. The egg and sperm combine to make an embryo.
If an abnormally shaped sperm fertilizes an egg, does that increase the chance of genetic abnormalities? There is no known scientific relationship between the shape of sperm and congenital disabilities. However, if the abnormality of the sperm is due to a genetic disorder, then the male’s descendants may inherit the same abnormal sperm morphology.
Semen analysis is heavily dependent on the observer and, therefore, can be variable and difficult to interpret. At least two semen analyses with at least four months between tests are recommended.
Author: Karen Synesiou, Infertility Portal, Inc.